Uncommon Symptoms of Endometriosis, And Why
Cold’s are known for congestion, the flu with a fever, infection with pain and swelling, and endometriosis with … 1000 symptoms that don’t line up the same with every patient. Some have pain with menses, others pain with sex, and some have no cyclical pain at all but suffer from seemingly unrelated issues like GI distress. Some have no symptoms at all and only discover advanced-stage endometriosis once they have trouble conceiving.
What gives?
A researcher once said, “Studying endometriosis is like nailing Jell-O to a tree.” (Donna Vogel, MD, Ph.D., 2000). It’s one of the most accurate quotes I’ve heard about the disease. Researchers in the lab, surgeons in the hospital, and the vast array of health practitioners working with endometriosis every day would agree: nothing is straightforward about this disease.
Today, let’s unravel a bit more about why endometriosis is so enigmatic and discuss some of the most uncommon symptoms of endometriosis.
Why Are Endometriosis Symptoms so Varied?
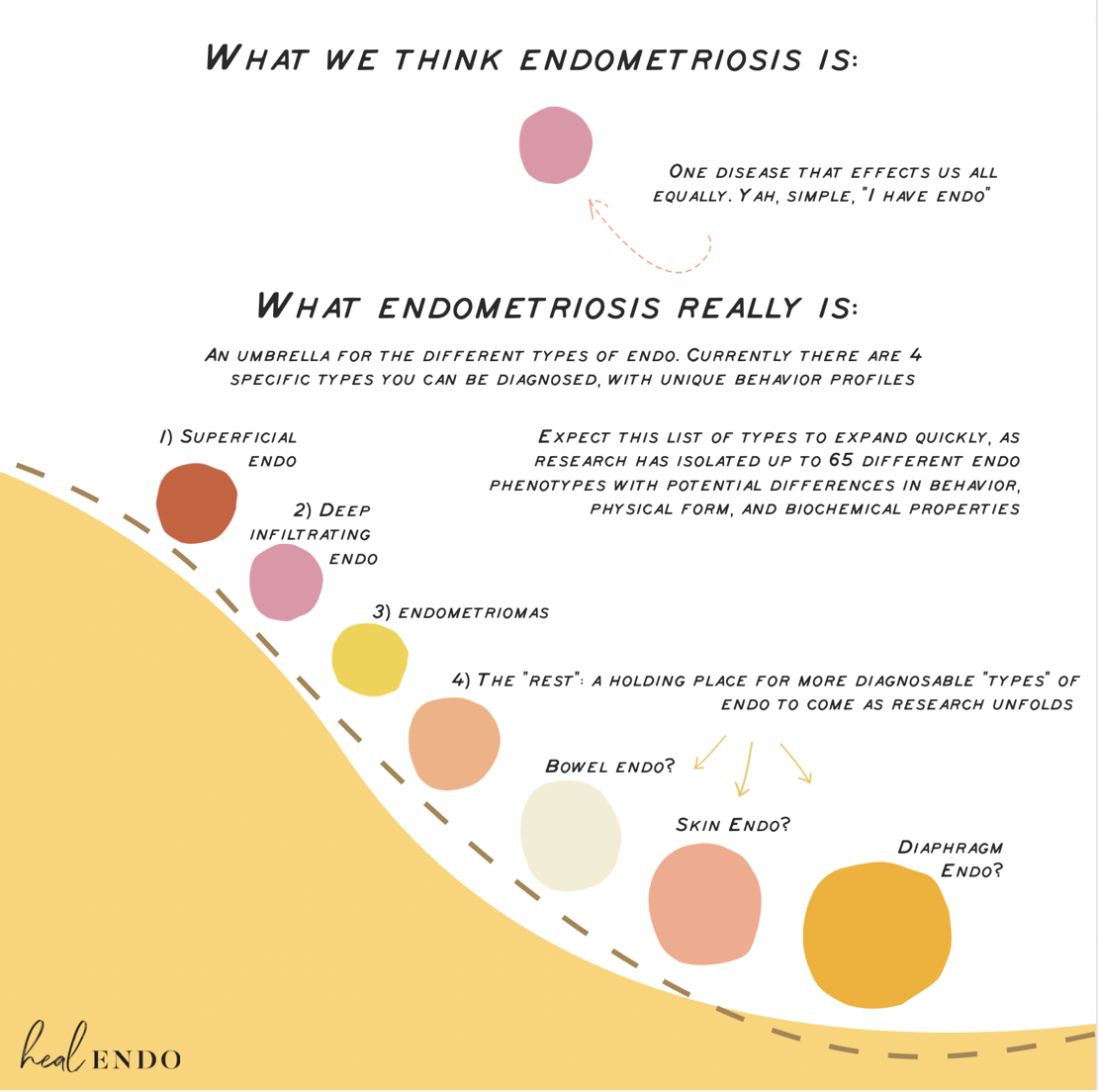
One of the reasons endometriosis is so hard to pin down on “normal” behavior is that it’s not a straightforward disease. As I discuss in my endometriosis book, it behaves similarly to cancer (albeit, one that doesn’t kill you), with many different varieties (65 and counting). This is why some endometriosis may be associated with pain or infertility or why some endo progresses rapidly while others are slow-growing or more likely to stabilize or regress.
Along with these factors of how endometriosis behaves on its own, our unique genetic footprint will contribute to different behaviors and symptoms. Some of us may be genetically predisposed to suffer more nervous system damage from endo pain, while others may develop far more scar tissue and adhesions than another.
It’s kind of like disease roulette, where you roll the dice on how a) the disease you get combines with b) your genetic lineage to c) produce your pathology and symptoms.
When you look at endo from this perspective (rather than as one disease that affects us all the same), we can better understand why symptoms vary so much.
The Most Common Symptoms of Endometriosis
You may be able to relate to some of the most common signs and symptoms of endometriosis, including the following:
Pelvic Pain. While pain is not everyone’s main symptom, for many it is. It may occur at menses, ovulation, randomly or constantly, with sex or physical activity, urination, or defecation—which is obviously different from solely being “period pain.”
Bloating, IBS, and GI distress. The severity of digestive woes we experience in the endo community is so common that there is a slang term for it: endo belly. Not to mention that many of us will receive either a misdiagnosis or a co-diagnosis with Irritable Bowel Syndrome (IBS). If you have endo, chances are that you also suffer with issues ranging from uncomfortable bloating to life-altering GI tract distress.
Hormonal imbalances. There is often a link among thyroid, adrenal, and sex hormone imbalances in the endo sufferer, and many of us suffer from accompanying symptoms that can include anything from personality-changing PMS to weight gain, excess facial hair, cold extremities, heavy periods, and more.
Fatigue. Chronic fatigue is a reality for many sufferers. Very different from just feeling tired, those suffering from chronic fatigue may not be able to even take a shower or prepare food without energy-regulation troubles.
Immune issues. Those with endo often suffer from allergies, getting sick often, rashes, colds, feeling rundown, or asthma—as well as autoimmune diseases. A whirlwind of immune dysfunction with endo.
Depression and anxiety. There is a strong link between having endo and mental health challenges, such as anxiety, depression, or even suicidal thoughts. According to a recent poll, nearly half of those with endo who experienced symptoms had suicidal thoughts.
Infertility challenges. It’s estimated that about 1 in 3 of us will deal with endometriosis-related infertility (although please note, this does not imply that 1 in 3 of us will never go on to have children). If you have been trying to conceive for over a year without success, and other issues have been ruled out, you should consider seeking an endo diagnosis even if you have no other symptoms. Endo is sneaky like that.
Uncommon Symptoms of Endometriosis
“Uncommon” would be considered the symptoms most people generally do not associate with endometriosis, although many specialists would (since they see such complex cases). They may be truly rare, or not, but the overall agreement is they’re not often listed as textbook symptoms.
To get an accurate snapshot of what sufferers deal with, I asked folks on my endometriosis Instagram what their most peculiar symptoms were. I received an avalanche of symptoms, many truly heartbreaking. Although I couldn’t fit all the comments in here (read the post though, if you want to see them!), I did my best to strategically organize these symptoms into categories, along with some potential reasons why.
Cyclical Chest, Rib, and Shoulder Pain
“Sharp breast/chest pains from the front all the way to the back. Like an arrow went through my body”
“Burning rib cage pain, presumably from lesions that were up high in my abdominal cavity”
“I knew I had endo because I’d get a sharp pain in my right rib area every time I was menstruating—like clockwork. Confirmed diaphragmatic endo. Much better after excision surgery.”
“I had a jabbing pain under my right rib during the heaviest part of my cycle. Of course, doctors just thought that I had pulled a muscle or had to poop. I had one doctor say that would be too rare to have endo under my rib. During my excision surgery, they found lesions under my right rib.”
Why? Thanks to “referred pain”, this symptom may be due to endo high in the abdomen, lungs, liver, or on the diaphragm. Referred pain is a sensation of pain radiating from where the trigger actually is to somewhere else in the body. If you’ve ever had a deep tissue massage, for example, and felt pain in your neck when she was massaging a not your back, this is the same thing. So, if you have this type of pain, definitely connect with an endo specialist surgeon (not your local OBGYN), who can start to help you find relief.
If you have this pain, but it’s not cyclical, it may not be endometriosis. It could be tight shoulders, weak core, posture, etc. Reach out to a physical therapist who can help see if your issue is structural.
Cyclical Sciatica, leg Pain, or foot Pain
“My right food would always go numb and the lower leg would feel engorged (I don't know how else to describe the feeling). Inserts irritated my arch and the right pant leg would always feel too tight. This passed after endo surgery, so I can only assume it was endo-related.”
“Right hip and leg pain, deep in the hip socket a week before my period, sometimes it’s challenging to bear weight.”
“Horrible pain in my hands, shoulders, and neck when my period was coming, low fever in ovulation and beginning of period, sensitive skin like it was burning, and allergies to moisturizer, cold legs, pain in joints and hips, my legs will be very tight ( like I was walking in water instead of the floor)”
“Right groin pain, leg pain, and sometimes inside foot pain during ovulation, discovered I had endo on the right side pelvis at uterosacral ligaments and sciatic nerve, never had it again after surgery.”
“For the last 8 months, I have gotten sciatica down my left leg only and only in the side of my thigh with every period. Sometimes, it’s my first clue that my cycle is starting. Hurts bad for 2 days and then gets better.”
“Lower back pain that curved around the front of my thigh and shot down to my knee during period. Also noticed white specs on my nails from lack of zinc”. [Read this to find out how zinc deficiency is associated with endometriosis]
Why? When this pain is cyclical, there is the potential for endometriosis on the sciatic nerve. This totally happens and should be investigated by a specialist for you to find relief! Foot pain may be a referred pain issue from lesions near nerves that stimulate pain in the foot.
Beyond endo lesions themselves, pelvic floor dysfunction, inactive glutes, and poor posture can all contribute—many issues those of us with endo (and chronic pain) have. One patient also mentioned the place in her foot that hurt was the “pelvic” location in foot reflexology. Working with holistic practitioners (such as body-workers, acupunturists, etc) may really help
Bladder Pain
“Intense bladder pain and pressure when my bladder was full (so especially felt when awaking each morning) and a shadow of the pain remaining for half an hour after emptying my bladder.”
Why? Endometriosis can grow on the bladder. If you have cyclical bladder pain or blood in your urine, it’s important to check out! If your bladder pain is consistent month round, you should also investigate interstitial cystitis or mast cell activation syndrome, both of which can create pain. Last, pelvic floor dysfunction and intra-abdominal pressure can increase pressure on the bladder, causing pain, pressure, or leakage. You could be suffering from any/all of these issues, so make sure to investigate each one!
Ovulation Pain
“When I ovulate, it feels like my ovary explodes. Every time.”
Why? Ovulation pain is pretty common in the endometriosis community, but so few people talk about it! Of course, it can be due to endometriosis growing on an ovary. A clue to this may be that one ovary hurts more than another every other month.
However, I personally had terrible ovulation pain, and no endo on the ovaries. How come? This ovulation pain can be due to histamines or MCAS since heightened estrogen levels at ovulation (when they peak) can trigger mast cells, which create a wave of pain-provoking histamines and other symptoms. These histamines are associated with pain and damage in the endo body, and not something to take lightly. Diet and lifestyle are important factors to consider here, investigating MCAS or histamine sensitivity issues, and checking in on hormone levels since estrogen dominance can play a big role as well.
Joint or Nerve Pain
“Joint pain in both hands, fingers, and wrists with stiffness, worst before and during the period.”
“Having an arthritis flare that shows up with PMS and then magically disappears after day 2 of my period.”
“I experience a lot of feet and hand numbness/tingling. Tingling in my face and scalp.”
Why? When estrogen drops during the luteal phase and on your period, it can cause arthritis symptoms and joint pain. “Many young women with inflammatory arthritis, including psoriatic arthritis and rheumatoid arthritis, report flares in their symptoms when they have their period.” If you have a similar symptom, work with your doctor to ensure you’re not also suffering from inflammatory arthritis.
Tingling, skin sensitivity, etc may be the result of premenstrual dysphoric disorder (PMDD). PMDD is like is a PMS on steroids (like, way worse!). It’s considered a severe and chronic health condition that should absolutely be treated, and many of us with endo have it but chock symptoms up to endometriosis. Luckily, endometriosis diet and lifestyle approaches are a GREAT place to start for this.
Cyclical Flu-Like or Food Poisoning-Like Symptoms
“During PMS, especially the day right before menstruation I will get food poisoning symptoms. Nausea, diarrhea, cold sweat and shaking. One bite of food and my body gets upset.”
“Chronic sore throat, worst before and during the period.”
“Fever with every period and ovulation”
“I would get a cold or flu before each period started.”
Why? There is something called Period Flu. Before your period, the level of inflammatory chemicals called prostaglandins increases to help shed the uterus lining. Prostaglandins also rise when there is a viral, bacterial, or other pathogen infecting the body, or when there are other inflammatory triggers. So if you’re dealing with a LOT of inflammatory triggers, and then add in your cycle, your immune system will send out a lot of prostaglandins. This can set off a systemic inflammatory response, just like you would get with the flu, including flu-like symptoms and fever. This can all be made even worse by estrogen dominance (and progesterone deficiency or resistance). Like PMDD (as mentioned above), endometriosis diet and lifestyle can play an enormous part in managing symptoms. Additionally, some women feel this symptom totally disappears after surgery.
Allergies, Rashes, heart rate changes
“I had cyclical shortness of breath and cyclical changes to my heart rate. My heart rate would drop into the 30s when sitting during certain times of my cycle. The shortness of breath has completely gone away since my excision surgery. I still have cyclical heart rate changes, which are much less frequent.”
“Terrible allergies that went away after surgery. I mean, vanished. I had no idea they were related”
“At stage 4 and frozen pelvis, I developed what I thought was POTS: random episodes of high heart rate upon standing or any exertion and feeling out of breath. I also developed weird rashes that would sometimes itch on my legs and the sides of my hips that would come and go. I had a terrible pain run from my pelvis down the left side of the hip and started cyclically. Eventually, it was almost all the time to the point I couldn’t walk and almost got a wheelchair. Once I had a total hysterectomy with ovaries too, everything went away, and I’ve never had these again.”
“Rash on my stomach, always when ovulating.”
“Itchy skin and hives. I'd get itchy bumps, similar to mosquito bites, around my period. I'm guessing some kind of histamine reaction brought on by hormones.”
Why? Many women with endo suffer from allergies. This may be in part thanks to the heightened immune response associated with endo, but also thanks to endo lesions themselves! Endometriosis lesions are chock full of mast cells, those little buggers that produce histamines, a chemical that makes us swell, itch, and inflame. It’s why endometriosis is associated with histamine sensitivities as MCAS (Mast Cell Activation Syndrome), and MCAS is associated with allergies, rashes, heart rate changes, flu-like symptoms, and often painful ovulation as well. If any of these stand out for you, look more into MCAS and/or histamine intolerance. For some of us, the symptoms may only be relieved by surgery since the lesions can be such a powerful instigator/contributor.
Breathing Issues
“Cyclical shortness of breath and cough.”
Why? There is a possibility for endo in the lungs, which may cause cyclical breathing issues, cough, or coughing up blood. Beyond that, there’s the possibility of hormonal fluctuations triggering anxiety, which can lead to a feeling of shortness of breath.
Irregular Vaginal Bleeding
“Long period and ovulation spotting”
“I had my period for four months straight.”
Why? Some women with endometriosis may have bleeding or spotting throughout their cycle, not just with their period. This can be due to extreme hormonal fluctuations, bleeding cysts, or potentially adenomyosis. Hypothyroid is another potential culprit, which is associated with endo (as in you’re more likely to get it if you also have endo). This can be easily tracked by your doctor with blood tests.
Cyclical Bleeding that was not Vaginal
“Blood in my nose (after blowing, not fully bleeding) for a week before my period”
“Bleeding from my belly button every period.”
Why? You can have endo lesions anywhere, including the nose, naval, and even skin. If you have cyclical bleeding like this, you should definitely have it checked out by a endo specialist.
One of my most annoying symptoms was a deep, nauseating “churning” feeling in my abdomen whenever my heart rate went up. When it settled again, the feeling went away. And, yes, FYI, that is Jason Mamoa.
Cyclical Tummy Troubles
“GERD for a week, only after my period.”
“Piercing sudden constipation pain only the day before my period would start, but being unable to have a bowel movement. I passed out from it at least once and several times was on the brink of passing out, but lay down fast enough to prevent it.”
Why? While general GI tract distress is a common symptom of endo, cyclical tummy troubles like this may be an indicator of endo growing on the bowel, or elsewhere. If it's not endo lesions, hormone imbalances may play a key role here since estrogen and progesterone levels can provoke tummy troubles cyclically as well.
Nerve and Muscle Involvement
“Weak and achy legs a few days before menstruation.”
“Peripheral neuropathy in all 4 extremities that directly correlate to pain/inflammation of my cycle.”
“I used to have back spasms every time I laid down. After the hysterectomy, the spasms stopped.”
Why? This may also be due to a hormonal imbalance and fluctuations during the cycle. When estrogen dips after ovulation to your period, it can trigger peripheral neuropathy, muscle weakness, and spasms in some people. It may also be associated with PMDD, as explained under Joint and Nerve Pain.
Everything Else Symptoms
"This is weird but my sweat would smell sour right before & during ovulation. It started when my normal endo symptoms got worse but once I had my excision surgery, my sweat smells like normal?”
“I would wake up in the middle of the night shaky and in a cold sweat super often, couldn’t sleep a full night, usually just 2 hours at a time. I think this was from not eating nearly enough bc I was having really intense digestive issues. Post surgery I’m back to normal sleep.”
“Fainting during ovulation.”
“Dizziness and feeling blood circulation leave my extremities and like about to pass out early morning on first day of menses(like 4,5am) before full bleeding starts later in the day. Almost feels like what I imagine a panic attack would be like… but only on day 1.”
“Cyclical ulcers in the mouth and inside of the lips”
Personally, I developed this bizarre symptom that was debilitating for my mental health. Formerly an avid runner, surfer, and adventurer, I found that if my heart rate became elevated (through, like, any of my favorite activities), my internal organs felt like they were “churning,” similar to a feeling one might get before explosive diarrhea (luckily no diarrhea would come!. It was so awful and nauseating, and I ended up not being able to raise my heart rate. See ya running, surfing, and all fun things :( Luckily, this symptom went away after I started properly treating my endometriosis.
If you have a symptom that is not listed here, that’s okay. Remember, if you personally suffer from symptoms you haven’t seen listed anywhere, you’re not alone. Remember, endo is a full-body disease that affects us all differently!
Why so many symptoms?
One reason for this wide variety of pain symptoms is that endo lesions grow more sensory nerve fibers than normal tissue does. Sensory nerve fibers alert our brain to stimuli—they are how you know when you step on a sharp rock or have an itch on your arm. In a highly inflammatory environment, the high number of sensory nerves can send constant alert signals, leading to the various manifestations of endo pain that many of us have experienced: everything from stabbing sensations in the gut or pelvis to feeling as if someone is wringing your uterus out like a wet towel, to pulling, throbbing, burning, even itching.
Endo can also grow anywhere. So pain in the ribs or coughing as menses may indicate something like lung endometriosis. Pain with urination may indicate bladder endometriosis. Etc.
There’s also such a thing as referred pain that can make us feel confused about where pain is coming from. If you’ve ever had a deep tissue massage where the masseuse pressed on your shoulder and you felt a pain in your ribs (for example), that’s referred pain. Similarly, referred pain can happen internally. Pressing on a spot of your pelvic floor may make your ovary feel painful, or gas moving through the intestine may make you have shooting anal pain. So even though nothing is actually happening at these “random” sites, it can still feel like it.
Lastly, systemic inflammation associated with the disease can give us whole-body pain. In my case, it was my joints, others may have migraines or headaches, and still others can get skin pain or pain elsewhere.
To Note, Symptoms Can Be Directly Caused By Endometriosis … or Not
While many of these symptoms are associated with endometriosis lesions themselves, it’s important to note (for best treatment options) that some of them may not be. For example, some pain may be due to an anti-oxidant deficiency or pelvic floor dysfunction more than the endo, and why such factors as diet, exercise, and pelvic floor physical therapy can be so helpful in clearing symptoms.
GI distress or bloating may be provoked by the inflammation coming from endometriosis lesions or may stem from dysbiosis and small-intestinal bacterial overgrowth, factors that should be treated separately from endometriosis lesions.
Infertility may be due to scar tissue, adhesions, lesions, or cysts, or may also be due to anxiety, nutrient deficiencies, poor pelvic blood flow, or reproductive tract dysbiosis.
Consistent pain, fatigue, etc can also be caused by other conditions, from MS to fibromyalgia, hypothyroid to HPA axis dysfunction. If you consistently suffer from symptoms, consider they may not be endo at all. Continuing to seek another diagnosis may be warranted.
Yes, there are so many moving parts in the endometriosis body! That’s why I like to look through the lens of endometriosis as a whole-body disease that is also more than the lesions. Many factors in the body contribute to both endometriosis and symptoms beyond the lesions, all of which are important to address for whole-body health.
Disclosure: I am not a medical professional, and nothing in this post should be considered a substitute for medical advice. I do not diagnose conditions or make specific treatment recommendations through this blog or website. If you or any other person has a medical concern, consult with your health care provider.